Medical Billing Services Outsourcing and Impact on Medical Practices Revenue and Cashflow
Identifying the right diagnoses, writing prescriptions, or operating on patients is only a small part of what it takes to run a successful medical practice. There is also the aspect of managing the business side of things when it comes to operating a medical office, or really any business. You may guarantee that you will compensate for all of the services you provide by putting in place medical billing service procedures and then ensuring adherence to those procedures.
Medical billing services:
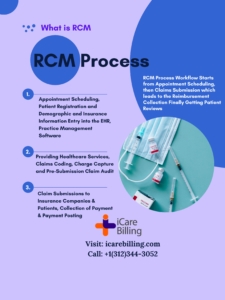
Your medical practices RCM activities start with scheduling the patient appointment and that’s the point from where you need medical billing services. You have an agreement with the patient and continue until the bill will pay in full. It could appear to be a lot at first, but if you break it down into smaller steps. You’ll find that it’s not quite as intimidating. In order to maintain your healthcare practice operational, one of the most important things you can do is ensure that the team with the right experience is on board to provide appropriate medical billing services.
The Processes Involved in Medical Billing Services
Here are a few critical processes that shall include in your medical billing service procedures. Whether you are just getting started with medical billing services or if you are wanting to improve your present system:
- Make a record of the patient in the EHR/EMR system.
- Check on the insurance eligibility and benefits verification.
- Document the details of each visit.
- Sharing your medical procedure details such as charting the billing team
- Add appropriate diagnosis and procedure codes
- Prepare medical claim
- Examine the claim.
- Payment and follow-up
- Prepare the patient statement
Develop a patient registration form:
Develop a patient registration form that compiles all of the essential information that you will require. Such as patient demographics, the patient’s referral provider, insurance identification, and any other necessary details. This data will be utilized during the subsequent visits, and the patient’s medical record will be kept current as circumstances warrant.
Verify the patient’s insurance information and coverage
Verify the patient’s insurance information and coverage before the appointment. And ask to see their insurance card to ensure that you have all of the necessary details. This step is necessary to ensure that there will be no unexpected charges further down the line. During subsequent visits, you will still need to verify that they have the same insurance data that will contain in your medical record and ensures the coverage eligibility with the insurance company.
Coders in the medical industry
Coders in the medical industry will make use of the medical clinical documentation in order to assign the codes. That is most appropriate for the services that will render. It is important to obtain a medical history during the first visit. And then monitor it for any changes during the following visits. The medical transcription will incorporate each and every one of these pieces of information.
Completion of the review of the medical notes, or transcription
Following the completion of the review of the medical notes, or transcription if the provider transcribes and doesn’t use the charting system. It will then prepare for delivery to your medical billers. Some healthcare providers handle the billing and coding on their own. While others contract out the work to a third party like medical billing services. Because of this, you need to make sure that the record of the visit is thorough and describes everything in detail. When this step of the process will complete, the charge entry process will be started to prepare the healthcare claim with the right diagnosis code, procedure code, date of service, and other necessary information to get the claim ready to transmit.
The medical claim will transmit:
Following this, the medical claim will transmit to the insurance companies, worker compensation, auto injury, or employer-funded insurance plans for the purposes of review and processing. Before sending the information to the insurance payers for reimbursement, the healthcare claim has to go through an internal audit generally known as “scrubbing,” during which any problems or errors that may have been applied will check for. Every medical billing company has its own rule-based engine to ensure the accuracy and completeness of the medical claim to avoid rejections. The claim scrubbing process is utilized to check the accuracy of each field in the claim HCFA-1500 Form or UB-04 form which also verifies each individual insurance requirement based on service type and the plan of care.
Review the claim and look for any discrepancies:
If the claim is rejected or denied, it needs to be checked if there are any errors or if the patient underwent any operations that were not covered by their particular insurance policy, if the policy was not active on the date of service, or if there is any incorrection information submitted on the claim. The majority of the time, insurance companies will provide an explanation for a claim that was rejected or denied so that any issues can be resolved.
The remaining balance (if any) will engage accounts receivable workflow to submit it to the patient, or financial granter once the claim will be processed or finalized by the insurance company and the final decision about reimbursement has been made. They will first generate a patient statement that explains the remaining balance along with reason or remarks, and then they will submit the invoice to the responsible party whether it is secondary insurance, the patient, or the financial granter of the patient.
Track down any past-due bills:
When the medical claim or bill is paid, this money-making cycle generally called RCM Process is over. Even so, you may require to track down any past-due bills, which is typically the most difficult part of the process for many medical practices that involve the whole denial management strategy. It is essential to take the help of medical billing companies that have experienced teams of medical billers in order to guarantee that you will be paid for the services that you provide. Sometimes heavy medical bills which are sent to patients as patient responsibility need a little more care from the billing team and healthcare provider end to ensure patients get the easy installment options with specific percentage write-offs as a professional courtesy in case they wanted to pay off the whole amount at once. This helps to retain the healthcare office’s clients (Patients) and on a practice level, keeps a steady cash flow.
Well-defined medical billing systems
It is important for your medical office to have a well-defined medical billing system run by an experienced medical billing company in place to assist guarantee that it runs smoothly. That will help to get reimbursed for all of the services that you perform in the healthcare facility. It is possible that getting everything organized will take a little bit of time, but in the long run, it will be well worth the effort.
It is simple to lose track of payments or to find oneself dealing with patients whose bills have not been fully paid. You can spare yourself a lot of hassles in the future by having an experienced and well-recognized medical billing company like “iCareBilling LLC” to properly set up your medical billing and collection processes and workflow in place. If you are facing difficulty in getting paid by the insurance company in a timely fashion, you can reach out iCareBilling to schedule a free medical billing consultation to learn more about how the current workflow can be improved. It might be challenging to maintain a steady cash flow by yourself because you have been trained for years to treat patients, not to manage the RCM side of your business. Let the experts handle this task so you can focus on patient care.